Health – Malaria
Malaria, the current situation in South Africa
In accordance with the South African National Guidelines for the Prevention of Malaria 2018, malaria prophylaxis is indicated for the prevention of malaria in non-immune travellers to malaria areas. The recommended medication is doxycycline, mefloquine and atovaquone / proguanil. Previously, all these prophylactics were freely available in travel clinics and pharmacies. Mefloquine (Lariam®) is the only prophylactic that is safe to use in PREGNANCY, provided the person has no other contra-indications to the use of mefloquine. Although pregnant women should not travel to malaria areas, travel is sometimes unavoidable due to personal circumstances. CHILDREN should also not travel to malaria risk areas and children under the age of five years are at particular risk. If travel is unavoidable they MUST take malaria prophylaxis.
- Mefloquine is safe to use in children that weigh more than 5kg, provided they do not suffer from any contra-indications.
- Children who weigh 11 to 40 kg can safely use the paediatric formula of atovaquone / proguanil, previously marketed in South Africa as Paediatric Malanil®
The Dilemma
- Mefloquine has not been available in South Africa since 2018 and
- Paediatric Malanil® has not been available since mid-2023.
- Adult formulations of atovaquone / proguanil (Malanil® / Mozitec® and Malateq®) can NOT be used in children as breaking the tablets does not provide a safe and / or reliable dose of the active ingredients. Suspending tablets in water is not a solution (SIC!) as the active ingredients do not dissolve equally leading to potential over / under dosing.
- Doxycycline can be used in teenagers and adults but should be used with GREAT CAUTION in younger children.
TRAVEL DOCTOR has obtained stock of mefloquine and paediatric atovaquone / proguanil (Malarone Junior® ) as Section 21 medication. It is available on consultation from our travel clinics in Rosebank and Northcliff in Johannesburg. As very few other sources stock these prophylactics due to low demand and a large administrative burden, we now make this available to all South African travellers on-line.
If you are travelling to a malaria risk region and you are pregnant or travelling with children and you would like to obtain mefloquine or paediatric formula atovaquone / proguanil, please note the following:
You will have to:
- Agree to an online consultation with one of our travel health nurses
- Complete a pre-travel consultation form online
We will contact you to conduct a brief consultation via Teams
Once the consultation is completed during which we will check for indications and contra-indications to the requested / proposed prophylactic and your delivery address, the tablets will be delivered to you by courier.
The Cost
Submitting your pretravel form for review does not cost anything.
Once your pre-travel form has been reviewed we will contact you by email.
We will provide you with a cost for your online consultation as well as the cost of the prophylaxis and courier fee.
You will be required to pay online via Netcash.
Once payment is confirmed we will agree on an online appointment time with you
On confirmation of what you need and that you understand how to use the prophylaxis we will courier the medication to you.
Delivery is in approximately three working days from the date of consultation.
Malaria Prophylaxis
Background
When considering malaria risk, travellers should bear in mind that NO Anti-malarial provides 100% protection against the disease. Thus, avoiding mosquito bites remains the cornerstone of protection against malaria. DO NOT GET BITTEN!
Although no Malaria Prophylaxis provides 100% cover, one should consider that 90% protection is better than no protection at all. Therefore, the use of Malaria Prophylaxis is highly recommended as a second line of defense against malaria.
There are various myths surrounding malaria prophylaxis ranging from Gin being a good substitute, to prophylaxis masking the symptoms from medical experts. To find out the truth about prophylaxis and its effects, travellers should consult their nearest Travel Doctor.
Myths and Truths
| Myth: | Gin & Tonic (G&T) works just as well as any prophylaxis. |
| Truth: | Gin (or any other alcohol for that matter) does not provide any protection against the malaria parasite. Tonic water (which contained quinine) however, was historically used as malaria prophylactic. Considering that Tonic water today contains extremely small quantities of quinine, one would need to consume G&T in units of multiple litres per hour to provide any significant level of protection. |
| Myth: | Prophylaxis makes the disease undetectable. |
| Truth: | Although malaria prophylaxis is supposed to eliminate malaria parasites, most modern laboratories can still detect the disease in the blood of a victim. In most cases a negative result with continued illness will warrant a second and third blood smear examination. In fact, the World Health Organisation (WHO) recommends 7 tests to completely eliminate the possibility of Malaria. If you suffer a malaria infection, it will be found, even while taking prophylaxis. |
| Myth: | All prophylaxis has the same side effects. |
| Truth: | Most travellers don’t suffer any side effects from prophylaxis. However, because we are each biologically unique, some travellers may experience side effects. Different anti-malarial tablets will have different side effects for those that experience them. The best choice of tablet should be made in consultation with a travel health specialist such as the Travel Doctor. |
| Myth: | Frequent travellers can become immune to malaria. |
| Truth: | People born in malaria-endemic areas become partially immune because of frequent infection, but the mortality rate amongst babies and toddlers remain extremely high. Travellers never become immune – in spite of frequently being infected – and they are in danger of dying every time they contract malaria. |
Prophylaxis Options
No malaria prophylaxis offers complete protection from the malaria parasite, but chosen and applied well, the combination can provide 90% protection against malaria illness and death. It has been shown that even if illness does occur, the likelihood of cerebral malaria is diminished, and the chance of death reduced significantly.
Options include: Mefloquine (Lariam), Doxycycline and Atovaquone & Proguanil.
Regimen
| Product | Before Exposure | During Exposure | After Exposure |
| Mefloquine | 1 week prior to departure | 1 tablet weekly | 4 weeks after |
| Doxycycline | 2 days prior to departure | 1 tablet daily | 4 weeks after |
| Atovaquone & Proguanil | 2 days prior to departure | 1 tablet daily | 1 week after |
The Disease
Malaria is a parasitic infection of the red blood cells. It is acquired via the bite of female Anopheles mosquitoes.
The epidemiology of the disease is complex, depending on factors such as altitude, climate (temperature and rain fall), mosquito-breeding sites and human behaviour for successful transmission of the disease.
There are five types of parasites namely P. vivax, P. malariae, P. ovale, P. knowlesi and P. falciparum. Vivax, malariae, ovale and knowlesi can cause serious illness, but seldom cause death in otherwise healthy patients. Plasmodium falciparum on the other hand can cause cerebral malaria and ultimately death in a relatively short period of time, if left untreated. Plasmodium falciparum (aka cerebral malaria) is the most prevalent malaria species in sub Saharan Africa and the anopheles mosquitoes (its distributor) can be found in most African countries.
All age groups are at risk of being infected with malaria.
Where the disease occurs
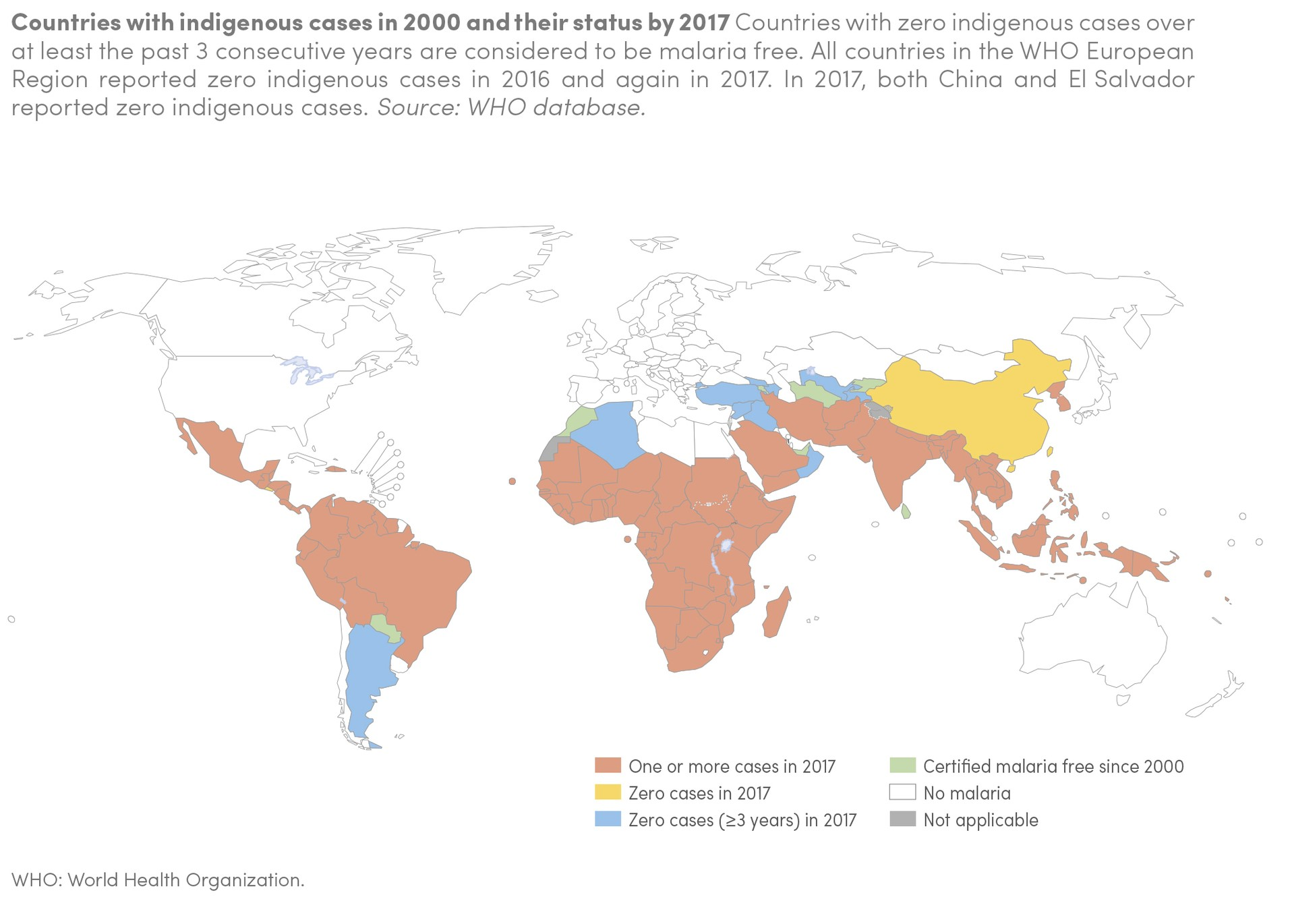
For those travelling to many of the warmer regions of the world there may be a risk of contracting malaria. Each year this parasitic disease causes many deaths both in the tropics and among travellers returning to their home countries. Most of the transmission occurs in tropical Africa (approx. 95%) with the rest in Asia and Central & South America.
Travellers need to remember that there is also a mild risk of the disease when visiting parts of North Africa and some parts of the Middle East.
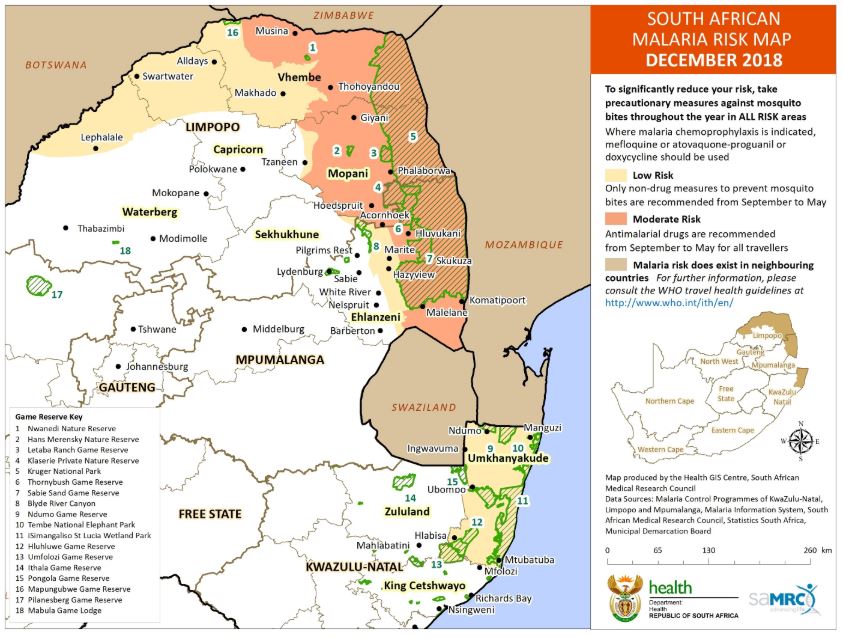
South Africa Risk Map:
Disease Transmission
In the majority of cases* the disease is transmitted to humans through the bite of an infected Anopheles mosquito. The parasite enters the blood and passes very rapidly into the liver cells. After an incubation period (usually 7 to 17 days**) the parasite breaks out of the liver and back into the blood stream. At this stage the infected red blood cell begins to break down and only then does the patient start to develop symptoms.
* The disease can also be transmitted through blood transfusion, infected needles and from an infected mother to her unborn baby.
** P. malariae usually presents between 18 and 40 days after a bite. The incubation period may be highly variable due to a variety of factors.
Malaria Life Cycle
Symptoms
There are no ‘typical’ malaria symptoms: All persons recently returned from malaria areas experiencing a ‘flu-like’ illness with symptoms that may include all or any of the following, should be considered to have MALARIA UNTIL PROVEN OTHERWISE:
- Fever and sweating
- Cold shivers
- Headache
- Muscle and/or joint pain
- Diarrhoea and/or vomiting
- Generalised flu symptoms
Suspected malaria represents a MEDICAL EMERGENCY and requires immediate medical consultation. Correct diagnosis and effective treatment depend on a comprehensive, detailed travel and exposure history, thorough clinical examination and reliable laboratory confirmation.
Diagnosis
It is possible to test yourself for Malaria with a rapid finger prick test supplied by the Travel Doctor.
While the rapid antigen tests are very reliable, they are not 100% accurate. Implying that a test might return a negative result, when in fact, the patient suffers a malaria infection.
One negative rapid test does not exclude malaria. Following a negative test, it is therefore important to repeat the test every four hours, until the patient’s condition has improved, or an alternative diagnosis has been made.
Fundamentally, the most accurate method of confirming a malaria diagnosis is through the microscopic identification of the parasite’s presence in a patient’s blood.
Protection
There are three golden rules for preventing illness and death from malaria:
1. DO NOT GET BITTEN:
- Avoid bites at all times in all malaria risk areas, but especially during or immediately after the rain season.
- The more mosquito avoidance measures used, the better.
- Cover up with long sleeves, trousers, socks and shoes. (90% of mosquito bites occur below the knees!)
- Apply DEET (diethyltoluamide) insect repellent to exposed skin every 4 hours.
- Only sleep in air-conditioned or screened accommodation or carry an insecticide-impregnated bed net – and sleep under it!
2. SEEK EARLY TREATMENT:
Any flu-like illness, (fever, shivers, headache, muscle aches, vomiting, even diarrhoea) commencing 7 days, and for up to 6 months or even longer, after leaving a malaria risk region, should be presumed to be malaria. This is regardless of whether you think you have been bitten and/or malaria-prevention drugs have been taken correctly or not. Seek expert medical care immediately and ensure that the clinical diagnosis is confirmed with a reliable laboratory diagnosis to include a malaria blood smear and/or rapid antigen test, preferably with a full blood count.
3. TAKE “THE PILL”:
Malaria chemoprophylaxis kills the malaria parasite before the traveller (who has no natural immunity to malaria and never acquires it in spite of repeated infections) becomes clinically ill. They act mostly on the parasites in the blood phase when the parasites exit the liver at the end of the ‘incubation period’. Malanil® / Malarone® /Mozitec® / Malateq® however, works on the liver stage shortly after being bitten. Chemoprophylaxis must therefore be commenced before entering the malaria area, to ensure that protective drug levels are reached and that the drugs are tolerated. Likewise, prophylaxis has to be continued for 4 weeks after leaving the area to ensure eradication of parasites still emerging from the liver. As Malanil® and its generics also acts on the liver stage of the parasites, it can be stopped seven days after leaving the malaria area.
Malaria Should be Taken Seriously
It is essential that all travellers realise that malaria is a very serious disease. It can cause death in an ill patient very rapidly, and no vaccines against the disease is available as yet. The primary responsibility for protection rests firmly with the individual traveller. Prescribed prophylaxis will assist in combatting malaria infection, but they do not provide complete protection.
Query Malaria
If you think you have malaria:
Remember that patients may develop malaria despite having taken all reasonable care with both personal protection against mosquito bites and prophylactic drugs. The disease may present many weeks after exposure. If you feel you may have malaria it is essential that you undergo a thorough medical examination and malaria blood smear as soon as possible. Ensure that the medical staff consider your history of international travel to risk areas, recently or in the distant past. If you return from overseas and experience fevers, sweating, shivering, aches and pains and other flu like symptoms you should seek medical advice as soon as possible. Malaria can be a serious disease if left untreated. It is wiser to assume you have malaria until proven otherwise.